Think about sex – if you want to win that grant
Major funding agencies around the world are pushing for sex and gender aspects to be meaningfully integrated into all stages of the research they fund, from study design to data analysis and dissemination. So it pays, literally, to give some extra attention to the sex-and-gender dimension of your research. Besides, doing so can not only give your research proposal that extra edge but also enhance the societal relevance and innovation potential of your research.
What is the sex-and-gender dimension of research (SGDR), and why should I care?
Initiatives aimed at increasing the participation of women in research teams, leadership positions, and evaluation panels are well established. More recent and less well-known are efforts—by funders and journals alike—to encourage scientists to address the sex-and-gender dimension of their research (SGDR). This recent push is not about getting more scientists to undertake sex-difference research or gender studies. It is about getting all scientists to view the work they already do (or propose to do) through a sex-and-gender-conscious lens. Depending on the nature and scope of the research, scientists are urged to consider and examine the influence that sex, gender, or both sex and gender, have on the research in question. And such considerations should permeate all phases of the research cycle, e.g., establishing research priorities, formulating concepts, selecting standards or models, designing studies, analysing and reporting data, and disseminating research results.
Learn to use the terms correctly
'Sex' versus 'gender'
'Sex' refers to biological differences between females and males, including chromosomes, sex organs, and endogenous hormonal profiles.
'Gender' refers to socially constructed and enacted roles and behaviors which occur in a historical and cultural context and vary across societies and over time.
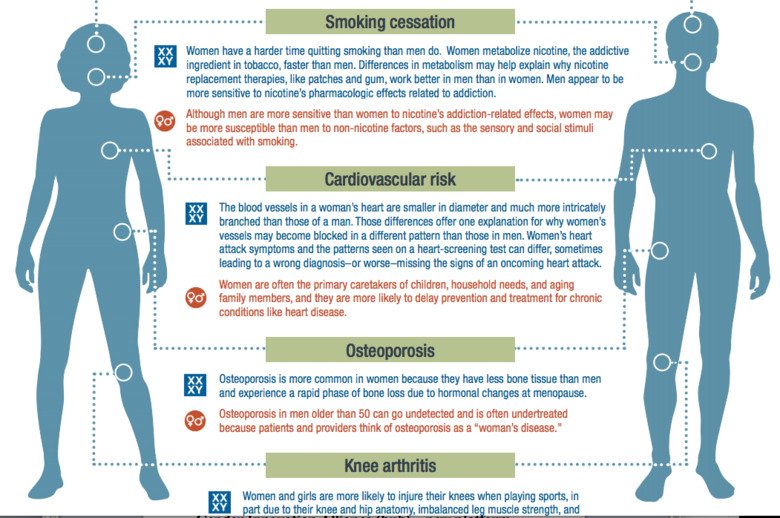
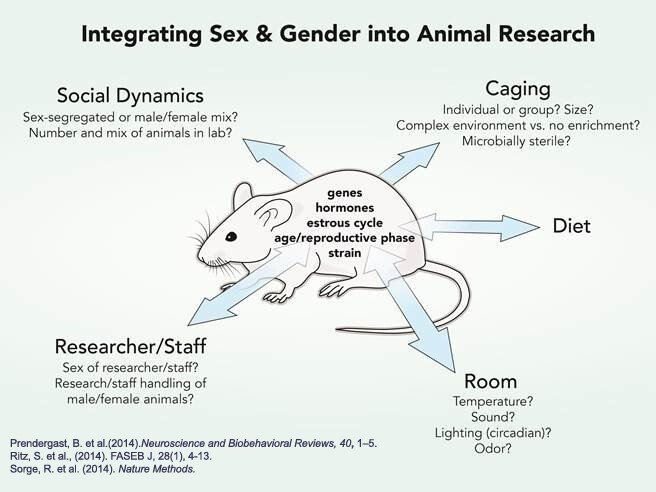
The continuous interplay between sex and gender (see definitions in the box above) has a profound influence on health and disease, and on access and response to healthcare. Taking sex and gender aspects into consideration should therefore form a fundamental part of biomedical research practice. Yet this is currently far from the case. While clinical researchers are increasingly aware of the importance of including women in clinical studies, women are often under-represented in clinical trials and the data collected is often not analysed or reported in a sex-disaggregated fashion. Moreover, basic and preclinical researchers more often than not rely on male (to the exclusion of female) animals, tissues, and cells. This over-reliance on the male can obscure important sex differences in processes of health and disease, as well as in response to treatment. So can failing to spot sex differences when using models or material of both sexes. Understanding these differences at the preclinical stage is vital to designing follow-on clinical trials appropriately—and vital, ultimately, to men and women’s health. As a stark reminder of the societal costs of failing to recognise sex differences in biomedicine, 8 of the 10 drugs withdrawn from the US market between 1997 and 2000 posed higher health risks for women.
Not only can failing to consider sex differences incur great health risks and societal costs, but it can also result in missed opportunities for discovering important mechanisms of health and disease. Indeed, a number of fascinating discoveries have been made when taking into account sex and gender variables. Comparing the sexes can uncover factors that protect against or contribute to disease, or reveal qualitative differences in the way males and females respond to stimuli. Pain research is a prime example, in which studying both sexes led to the discovery that males and females use different biological pathways and cell types in processing pain, with important implications for treating pain in men and women. Of course, not all traits, genes, or biological processes have sex differences; the key is to design studies that can capture variation both within and between sexes and to disaggregate data on the basis of sex, so that sex differences can be spotted should they exist.
At the other end of the biomedical spectrum, another often-neglected aspect is the role that gender plays in diagnosis, access to healthcare, implementation of health regimens, etc. For instance, autism spectrum disorder and attention deficit disorder present differently in girls than in boys and, as a result, are often undiagnosed or misdiagnosed in girls and women. Likewise, women with atrial fibrillation receive less anticoagulation treatment with warfarin than men do, even though they have a greater risk for stroke than men, while osteoporosis and depression are possibly underdiagnosed in men. Gender-sensitive medicine is not about considering the specific needs of women, but rather about considering the possibly different needs of both men and women.
Besides helping to avoid healthcare pitfalls, addressing the SGDR can also open up new opportunities in healthcare. By integrating the SGDR in your research and innovation you can not only enhance the societal relevance of the knowledge, technologies, and innovations you generate but also contribute to the production of goods and services that are better suited to potential markets.
What is the funder's perspective?
Recognising the importance of the SGDR, a variety of international, national, and private funding organisations—including the European Commission, the Swedish Research Council, the US National Institutes of Health, the Canadian Institutes of Health Research, the Research Council of Norway, and the Irish Research Council—require grant applicants to address the SGDR of their proposed research. Click on this link to find out about the specific SGDR requirements and expectations of major funding organisations.
A growing number of scientific journals, such as Nature, The Lancet, PLOS Biology, and PLOS Medicine, is likewise embracing this trend. So, competently addressing the SGDR can help you to not only fund your research but also get it published.
How can I integrate the SGDR in my research (proposal)?
General guidance
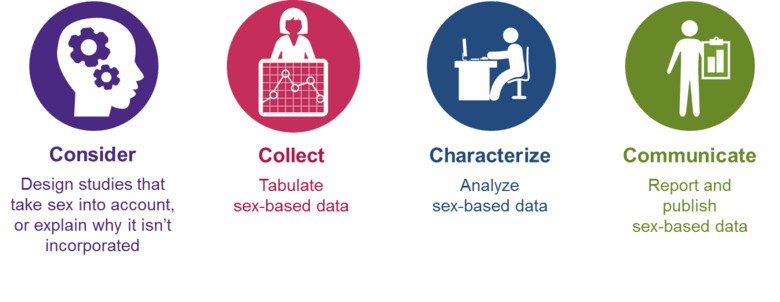
Familiarise yourself with the various methods of sex and gender analysis as you consider your research priorities, formulate concepts, determine standards or models, design studies, analyse and report data, and disseminate project results.
Below is some general guidance about considering sex as a biological variable in biomedical research and clinical care -- see 'Applying the new SABV (sex as a biological variable) policy to research and clinical care' for more details.
In biomedical research:
- Do a careful literature review: Are there known sex differences or gender disparities in the area of study? Add the terms "sex", "gender", "male" and "female" to your literature search. In addition to PubMed, use the GenderMed database.
- Randomise and balance the sexes in the study and control groups.
- If you are testing a pharmaceutical, consult the FDA Drug Trials Snapshots web page or the Janusmed Sex and Gender web page.
- If sex or gender differences are suspected, conduct pilot studies to determine whether powering the study to detect sex or gender differences is warranted.
- In analysing your data, regardless of whether or not the study was powered to detect sex differences, disaggregate the data on the basis of sex to see whether there are differences that are hidden when data from males and females are pooled. Analyse key relationships from males and females separately.
- Always report the sex of the cells, tissues, animals or subjects you are studying, and consider discussing possible sex and/or gender implications of your findings. If studying one sex only, justify doing so and note any limitations in your discussion.
See 'Studying both sexes: a guiding principle for biomedicine' for useful study designs and experimental approaches to considering sex as a biological variable.
Sex differences to keep in mind in clinical care/research:
- Symptoms: Men and women may experience different symptoms of the same disorder and report them differently.
- Medical history: For women, pregnancy should be included in the medical history.
- Physical exam, lab values and diagnostic test results: Some norms for standard lab values, etc., differ between men and women.
- Diseases and disorders: Prevalence of many diseases and disorders differs between men and women.
- Treatments: Women metabolise drugs differently and sometimes require lower doses than men. Drugs may also affect men and women differently.
If the SGDR is especially important to the research question or call for proposals, consider engaging scientists with gender expertise among your key research staff and/or including gender-dimension training in your proposal. Costs for such are often eligible for funding.
Good for science, good for society, good for you!
Ultimately, taking sex and gender into account in research projects is simply good scientific and ethical practice, contributing to rigour, reproducibility, and excellence in science and healthcare. Besides, applying a sex-and-gender perspective enhances the societal relevance of your research as well as its innovation potential. It’s a win-win!
